The Rinne test represents one of the most fundamental and enduring diagnostic tools in modern otolaryngology, serving as a cornerstone for evaluating hearing loss across diverse clinical settings. Heinrich Adolph Rinne (1819-1868), a German otologist, proposed the test, subsequently named after him, and it has remained virtually unchanged in its essential methodology for over 150 years. This simple yet powerful assessment technique continues to provide invaluable insights into the nature and extent of hearing impairments, making it an indispensable component of routine clinical examinations.
Understanding the Rinne test’s principles, proper execution, and accurate interpretation is crucial for healthcare professionals across multiple disciplines. From primary care physicians conducting initial screenings to specialists determining surgical candidacy, the Rinne test offers a rapid, cost-effective method for distinguishing between different types of hearing loss. Its enduring relevance in an era of sophisticated audiometric technology speaks to its fundamental utility and diagnostic accuracy.
What is the Rinne Test?

The Rinne test is a clinical diagnostic procedure that compares air conduction hearing with bone conduction hearing using a tuning fork, typically set at 512 Hz frequency. The Rinne test differentiates sound transmitted through air conduction from those transmitted through bone conduction via the mastoid bone. This comparison provides critical information about the integrity of the outer and middle ear structures, helping clinicians identify conductive hearing loss patterns.
Named after Heinrich Adolf Rinne, a German otologist who developed the technique in the 19th century, the Rinne test utilizes a tuning fork to evaluate the comparative efficiency of bone conduction (BC) versus air conduction (AC) in hearing. The test’s fundamental principle relies on the physiological fact that in normal hearing individuals, air conduction pathways are more efficient than bone conduction pathways for sound transmission to the inner ear.
The test’s elegance lies in its simplicity and the wealth of diagnostic information it provides. By leveraging the natural acoustic properties of sound transmission through different mediums, the Rinne test can quickly identify disruptions in the mechanical conduction system of the ear, providing immediate clinical insights that guide further diagnostic and therapeutic decisions.
The Science Behind Sound Conduction
To fully appreciate the Rinne test’s diagnostic value, understanding the basic mechanisms of hearing is essential. The external ear collects sound vibrations from the air and focuses these sounds onto the tympanic membrane. The ossicular chain (malleus, incus, and stapes) transmits vibrations through the middle ear. The stapes transmit these vibrations to the cochlea through the oval window.
Air conduction represents the normal pathway for sound transmission. Sound waves travel through the ear canal, causing the tympanic membrane to vibrate. These vibrations are amplified and transmitted through the ossicular chain to the inner ear, where hair cells convert mechanical energy into electrical signals for neural processing. This pathway provides optimal sound amplification and frequency resolution under normal circumstances.
Bone conduction bypasses some or all of these and allows the sound to be transmitted directly to the inner ear albeit at a reduced volume, or via the bones of the skull to the opposite ear. This alternative pathway becomes particularly important when air conduction mechanisms are compromised, serving as a backup route for sound transmission that the Rinne test specifically evaluates.
Step-by-Step Rinne Test Procedure
Pre-Test Preparation
Before conducting the Rinne test, several important considerations ensure optimal results. The examiner should use a 512 Hz tuning fork. One should avoid using a 128 Hz or 256 Hz tuning fork, as these are used to assess vibration sensation in neurological examinations. The room should be reasonably quiet. Patient comfort and cooperation are essential, particularly when examining children or anxious patients.
The choice of tuning fork frequency represents a critical decision. In a study of 200 patients with known air-bone gaps, we found that the 256-Hz tuning fork was more sensitive than the 512-, 1024-, and 2048-Hz tuning forks for discriminating conductive from sensorineural hearing deficits. However, the occurrence of false-positive responses limits its usefulness. Therefore, we believe that the 512-Hz tuning fork should become the standard tuning fork used in performance of the Rinne test.
Testing Procedure
The actual test involves two distinct phases that must be performed in proper sequence. Initiate the tuning fork’s vibration and then place the vibrating tuning fork onto the patient’s mastoid process of the tested ear. Ask the patient to cover the opposite ear with their hand. Ask the patient to report when the sound can no longer be heard.
Without delay, the still-vibrating tuning fork is then positioned 1 to 2 cm from the auditory canal. The patient again indicates when the sound ceases, and the time is noted. This immediate transition from bone conduction to air conduction testing is crucial for maintaining the integrity of the comparison.
The positioning of the tuning fork during air conduction testing requires particular attention to detail. Recent research has highlighted the importance of proper angulation and distance. The reliability of the Rinne test can be considerably impaired by incorrect positioning of the TF next to the ear. Not paying attention to the precise angle at which the tuning fork is held relative to the ear increases the potential for negative or equivocal results.
Interpreting Rinne Test Results
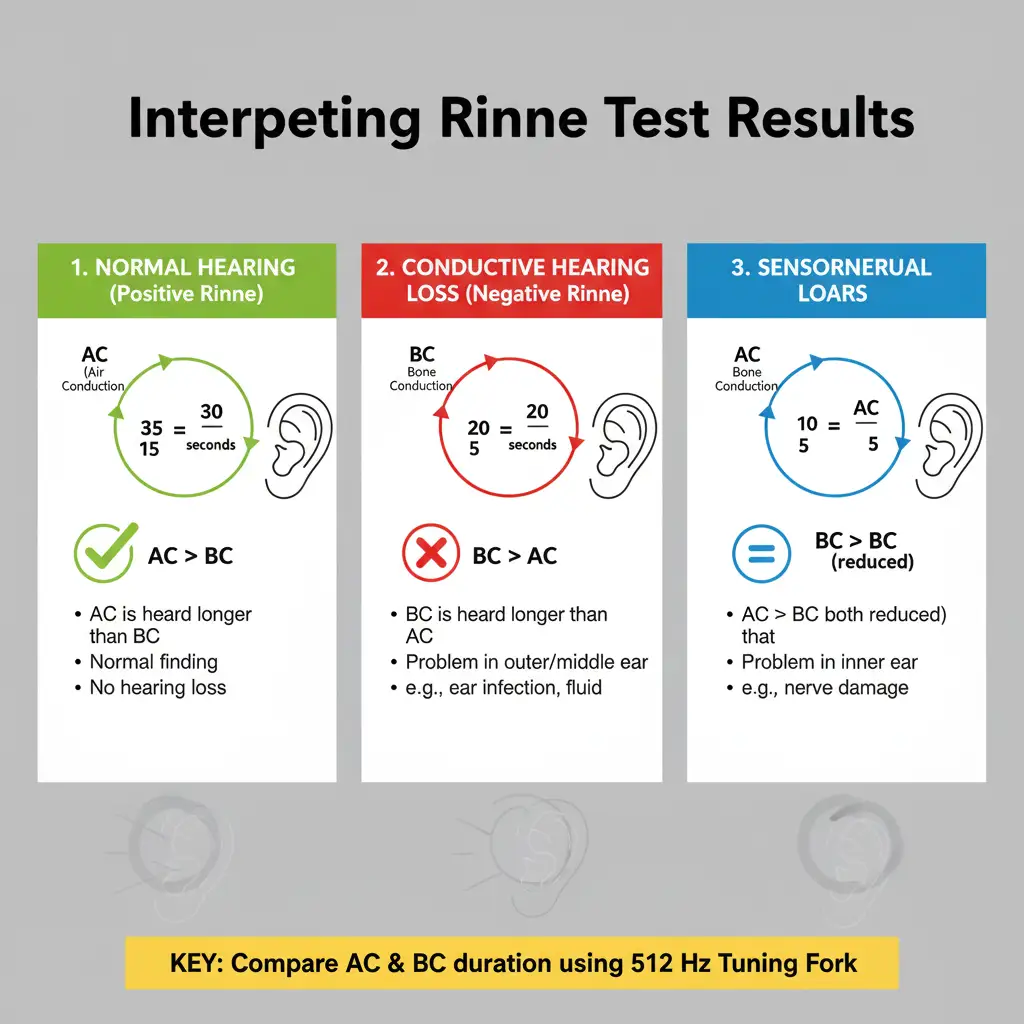
Normal Results (Positive Rinne Test)
The duration of sound perception via air conduction should ideally be twice as long as that through bone conduction. For instance, if bone conduction is perceived for 15 seconds, air conduction should be audible for about 30 seconds. This normal finding is termed a “positive” Rinne test, though this terminology can be confusing for clinicians.
Air conduction should be greater than bone conduction, so the patient should be able to hear the tuning fork next to the pinna (outer ear) after they can no longer hear it when held against the mastoid. This normal result is paradoxically called a positive Rinne test (as a positive medical test usually indicates an abnormality). This counterintuitive terminology has led some practitioners to avoid using positive/negative descriptors altogether.
Abnormal Results (Negative Rinne Test)
A negative Rinne test, where BC>AC, signifies conductive hearing loss. In such cases, sound conduction through air is impaired relative to bone conduction, pointing to anomalies in the outer or middle ear, such as ear infections, fluid accumulations, or other obstructive conditions. This finding indicates that the normal air conduction pathway is compromised, forcing reliance on the less efficient bone conduction route.
If the patient is not able to hear the tuning fork after it is moved from the mastoid to the pinna, it means that their bone conduction is greater than their air conduction. This indicates there is something inhibiting the passage of sound waves from the ear canal, through the middle ear apparatus and into the cochlea.
Sensorineural Hearing Loss Patterns
In cases of sensorineural hearing loss, the Rinne test typically remains positive because both air and bone conduction are equally affected. In sensorineural hearing loss the ability to sense the tuning fork by both bone and air conduction is equally diminished, implying they will hear the tuning fork by air conduction after they can no longer hear it through bone conduction.
This preservation of the normal AC>BC relationship in sensorineural hearing loss is crucial for differential diagnosis and helps distinguish inner ear pathology from middle ear dysfunction. The combination of Rinne test results with Weber test findings provides a comprehensive picture of the hearing loss pattern.
Clinical Applications and Diagnostic Value
Primary Screening Tool
The Rinne test serves as an excellent initial screening tool for hearing loss in various clinical settings. A Rinne test should be done with a Weber test to detect sensorineural hearing loss. This combination provides a rapid assessment that can guide further diagnostic workup and referral decisions.
Weber and Rinne’s tests are reliable and useful tools for assessing hearing loss in older, verbal children. They help distinguish between conductive and sensorineural hearing loss and so are more useful in patients with unilateral hearing difficulty. The tests are particularly valuable in pediatric populations where cooperation with formal audiometry may be challenging.
Surgical Decision Making
In specialized practice, the Rinne test plays a crucial role in surgical planning. In some patients with otosclerosis, the Rinne test is performed to determine if the patient is eligible for stapes surgery. The degree of conductive hearing loss as revealed by tuning fork testing helps predict surgical outcomes and candidate selection.
The test’s utility extends beyond simple diagnosis to include monitoring treatment response and postoperative assessment. For patients with middle ear pathology, serial Rinne testing can track improvement following medical or surgical intervention, providing objective evidence of therapeutic success.
Educational and Training Applications
Medical education has consistently emphasized tuning fork testing as a fundamental clinical skill. These tests are now routinely taught in medical schools and performed regularly to assess patients with hearing problems. The hands-on nature of the examination provides valuable tactile and auditory learning experiences for students and residents.
Diagnostic Accuracy and Limitations
Sensitivity and Specificity Data
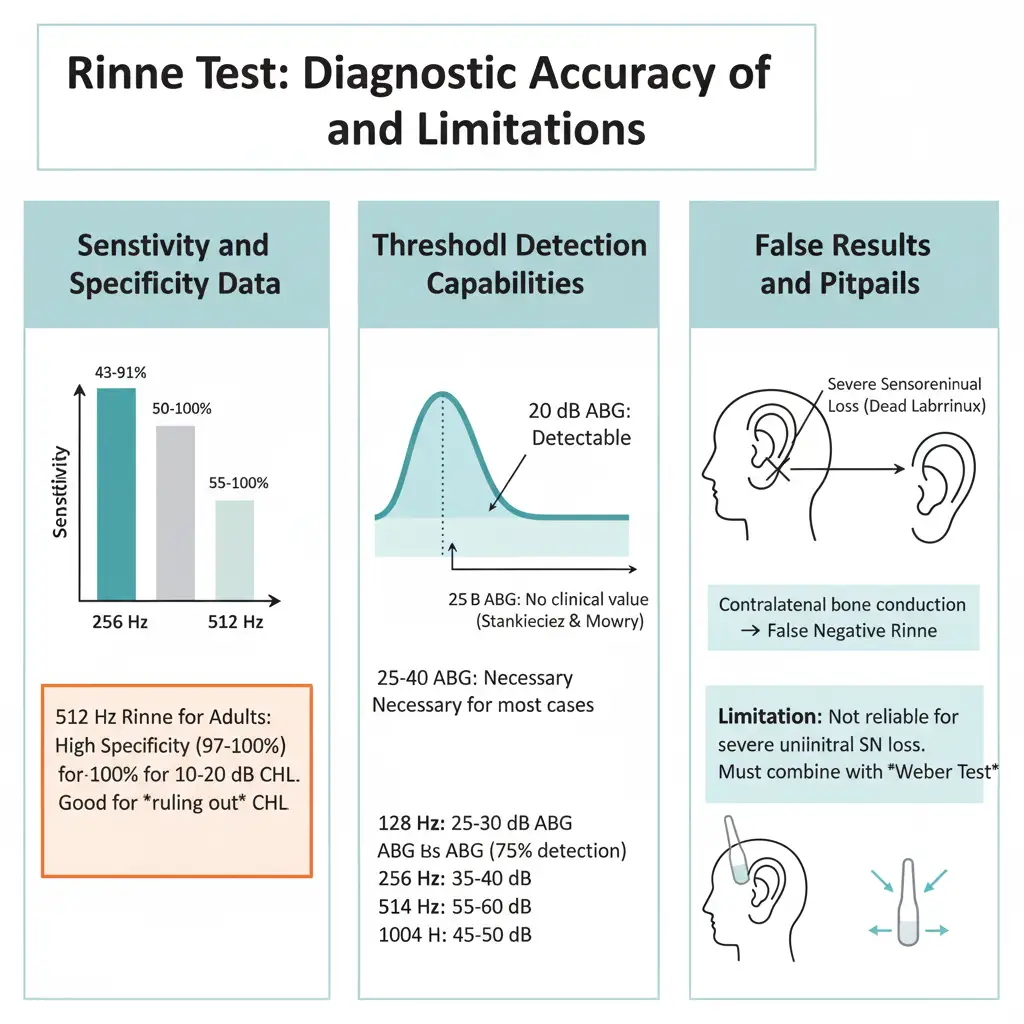
Recent systematic reviews have provided comprehensive data on the Rinne test’s diagnostic performance. The sensitivity and specificity of the Rinne test for detecting conductive hearing loss ranged from 43% to 91% and 50% to 100%, respectively, for a 256-Hz fork and from 16% to 87% and 55% to 100% for a 512-Hz fork. These variations reflect differences in methodology, examiner experience, and patient populations.
Among adult patients (who are most likely to have otosclerosis), the 512-Hz Rinne test had high specificity (97%-100%) and, thus, low false-positive rates for detecting at least 10 to 20 dB of [conductive hearing loss] CHL. This high specificity makes the test particularly valuable for ruling out conductive hearing loss when results are normal.
Threshold Detection Capabilities
The Rinne test’s ability to detect varying degrees of hearing loss has been well-characterized. According to Browning and Browning and Swan, the Rinne test can correctly detect conductive hearing impairment of 20 dB or more air-bone gap. The conclusion drawn by Stankiewicz and Mowry was that the Rinne test has no clinical value when the air-bone gap in the tested patient is less than 25 dB.
Air-bone gaps of 25 to 40 dB, depending on frequency, are necessary for the Rinne to identify the presence of conductive components in most cases. Gaps of 25-30 dB for 128 Hz; 35-40 dB for 256 Hz; 55-60 dB for 512 Hz; and 45-50 dB for 1024 Hz, are necessary for the Rinne to meet a 75% correct detection criterion.
False Results and Pitfalls
Understanding the limitations and potential sources of error is crucial for accurate interpretation. In case of a severe sensorineural hearing loss caused due to a dead labyrinth, a false negative Rinne test may occur. It is caused by the fact that even though one ear is unable to respond to the test, the other ear can still be stimulated by the bone conduction test.
The Rinne test is not reliable in distinguishing sensorineural and conductive loss cases of severe unilateral or total sensorineural loss. In such cases, bone conduction to the contralateral normal ear will be better than air conduction, resulting in a false negative. This limitation emphasizes the importance of combining Rinne testing with Weber testing for comprehensive assessment.
Modern Applications in Healthcare
Integration with Modern Audio Technology
While the fundamental principles of the Rinne test remain unchanged, modern healthcare has found innovative ways to integrate this classical assessment with contemporary audio technology. Just as noise-cancelling headphones offer benefits for audio quality in everyday listening, understanding sound conduction principles helps clinicians appreciate how different pathologies affect hearing quality and clarity.
The principles underlying the Rinne test also help explain why certain audio technologies are more effective for different types of hearing loss. For individuals with conductive hearing loss, bone conduction headphones can provide superior sound transmission by bypassing the damaged middle ear structures, directly stimulating the inner ear through bone vibration.
Digital Health and Telemedicine Applications
The COVID-19 pandemic has accelerated interest in remote healthcare delivery, including hearing assessments. While the Rinne test traditionally requires in-person examination, researchers are exploring modified versions that could be conducted remotely using smartphones and standardized audio frequencies. These adaptations maintain the core principles while expanding accessibility for preliminary screenings.
The integration of the Rinne test with modern wireless earbuds features represents an emerging area of interest. Advanced wireless audio devices with precise frequency control and bone conduction capabilities could potentially facilitate remote hearing assessments, though such applications require careful validation against traditional methods.
Frequently Asked Questions
What exactly does a positive Rinne test mean?
A positive Rinne test indicates normal hearing or sensorineural hearing loss. In this result, air conduction is better than bone conduction, which is the normal physiological state. The term “positive” can be confusing because it actually represents normal function rather than pathology.
How accurate is the Rinne test compared to formal audiometry?
The Rinne test’s accuracy varies depending on the degree of hearing loss and examiner experience. For detecting conductive hearing loss of 25-30 dB or greater, the test shows good reliability. However, it cannot replace comprehensive audiometry for precise diagnosis and should be considered a screening tool rather than a definitive diagnostic test.
Can the Rinne test be performed on children?
Yes, the Rinne test can be effectively performed on verbal children, typically those aged 4-5 years and older who can understand and follow instructions. The test is particularly useful in pediatric populations because it requires minimal cooperation compared to formal audiometry testing.
What tuning fork frequency should be used for the Rinne test?
The 512 Hz tuning fork is considered the standard for Rinne testing. While some studies suggest 256 Hz may be more sensitive for detecting conductive hearing loss, the 512 Hz fork provides the best balance between sensitivity and specificity while minimizing false-positive results from tactile sensation.
Why might someone get a false negative Rinne test result?
False negative results typically occur in cases of severe unilateral sensorineural hearing loss (dead ear). In these situations, bone conduction testing inadvertently stimulates the good ear through skull vibration, while air conduction testing only reaches the deaf ear, creating the appearance of better bone conduction.
How should the tuning fork be positioned during air conduction testing?
The tuning fork should be held 1-2 cm from the external auditory canal with the tines perpendicular to the ear canal opening. Proper positioning is crucial for accurate results, as variations in angle and distance can significantly affect sound amplitude and test interpretation.
Can the Rinne test detect all types of hearing loss?
The Rinne test is most effective for detecting conductive hearing loss. While it can identify sensorineural hearing loss patterns, it cannot quantify the degree of loss or distinguish between different types of sensorineural pathology. Combined testing with Weber test and formal audiometry provides more comprehensive assessment.
Is the Rinne test still relevant with modern audiometric equipment?
Yes, the Rinne test remains highly relevant as a quick, cost-effective screening tool that requires no equipment other than a tuning fork. It provides immediate results in clinical settings and helps guide decisions about further testing and referrals. Its portability and simplicity make it invaluable for initial assessments.